ISSN 2410-5708 / e-ISSN 2313-7215
Year 12 | No. 34 | June - September 2023
© Copyright (2023). National Autonomous University of Nicaragua, Managua.
This document is under a Creative Commons
Attribution-NonCommercial-NoDerivs 4.0 International licence.
Perinatal results related to altered Body Mass Index in pregnant women; systematic review
https://doi.org/10.5377/rtu.v12i34.16346
Submitted on Octuber 17th, 2022 / Accepted on April 25th, 2023
Renaldy Espinoza Sotelo
Student of the degree of Medicine and
Surgery at Redemptoris Mater Catholic University, Nicaragua.
Alexis Aguilar Meza
General practitioner. Redemptoris Mater
Catholic University, Nicaragua.
Fernanda Pineda Gea
General practitioner and hearing care professional.
Professor Redemptoris Mater Catholic University, Nicaragua.
René Alfonso Gutiérrez Aburto
Medical epidemiologist. Professor at
Redemptoris Mater Catholic University, Nicaragua.
Section: Health and Social Services
Scientific research article
Keywords: Pregnancy, Excessive gestational weight gain, Gestational BMI, Obesity and overweight, Perinatal outcomes.
Abstract
The altered BMI in women during pregnancy generates problems in perinatal results that harm the newborn as well as the mother herself. The study of the relationship between perinatal outcomes and altered BMI in pregnant women is a research area of growing interest, which has begun to be studied in the last two decades.
What is the available scientific evidence about body mass index in pregnant women and its perinatal effects?
Systematize the available and accessible medical literature on body mass index in pregnant women and its perinatal effects.
A systematic review of perinatal outcomes and their maternal-fetal effect was carried out. Nine scientific articles were included through the PUBMED metasearch engine, not including duplicate studies and published outside the study and search period, studies with poor methodological quality after applying the STROBE tool.
It was shown that obese and overweight pregnant women have a higher risk of cesarean delivery, fetal macrosomia in the newborn, and gestational diabetes. Pregnant women with excessive gestational weight gain according to IOM recommendations have a threefold risk of presenting preeclampsia and other fatal complications
There is a relationship between perinatal outcomes and the body mass index of pregnant women and it is extremely important to create strategies that reduce poor perinatal outcomes associated with an altered BMI during pregnancy.
INTRODUCTION: CURRENT STATUS OF THE TOPIC
Pregnancy is one of the most vulnerable stages in the life of women, in addition to having to go through the different phases of this biological period, incurs a nutritional risk due to the physiological changes of pregnancy, where there is an important anabolic activity that institutes an increase in maternal nutritional needs of almost all nutrients since the fetus develops at the expense of the mother. Among all these changes, weight gain caused by multiple factors such as the presence of the growing fetus, fluid retention, increased body fat, and increased uterine muscle mass stands out (Maldonado et al., 2008).
The recommended weight gain varies depending on the mother’s pre-gestational Body Mass Index (BMI), with greater weight gain in women with a low or normal BMI before conception than in overweight or obese women (Minjarez et al., 2014). Gestational weight gain (GPG) is a complicated phenomenon influenced not only by maternal physiological and metabolic changes but also by placental metabolism. In recent years, the Food and Agriculture Organization of the United Nations (FAO) and the World Health Organization (WHO) have proposed assessing the nutritional status of pregnant women using BMI, which is obtained by dividing the value of weight (kg) by that of height (m) squared.
Ramos et al. (2021) classify the increase in BMI into obesity and overweight, the first being body mass index (BMI) > 30 kg/m2 and overweight as a BMI of 25.0 to 29.9 kg/m2. The recommendations that are currently most accepted are those indicated by the IOM (Institute of Medicine of the USA), for weight gain about BMI before pregnancy (pre-BMI), in this way a pregnant woman with BMI in normal ranges should increase 11.5-16.0 kg, if she were overweight the increase should be between 7.0-11.5 kg and in obesity only 6 kg. Therefore, the increase in pre-BMI is related to obstetric events during pregnancy that can transcend after childbirth, Ramos et al. (2021, p.2) mention that among the main ones we can find: gestational diabetes (GDM), hypertensive disease, thromboembolic complications, cancer and adverse obstetric events (spontaneous abortion, infection, hemorrhages, anesthesia risks). In this way, we can say that the Body Mass Index associated with pregnancy has shown a good partnership with the degree of adiposity and with the risk of chronic non-communicable diseases such as gestational diabetes, and preeclampsia. macrosomia, prolonged deliveries, and higher rates of cesarean sections.
The above, objective of this research is to convey and emphasize the importance of the increase in BMI during pregnancy and its association with perinatal outcomes because most of the authors who have researched the subject conclude that maternal obesity contributes significantly to a worse prognosis for the mother and newborn during childbirth and in the immediate puerperium. The articles included in this systematic review agree that this increased risk is directly proportional and more severe to weight gain during pregnancy (De la Plata et al. 2018).
CLINICAL QUESTION and VARIABLES(PICO)
What is the available scientific evidence about body mass index in pregnant women and its perinatal effects? The PICO variables are broken down in the question posed above, which will govern the course of this review, which are below:
P-OBLATION: Pregnant women with altered BMI
I-INTERVENTION: Body Mass Index
C-OMPARISON: -------------------------
O-UTOCOME/RESULTS: Perinatal effects
MATERIAL AND METHODS:
Type of Study
The present research has a qualitative approach, its design being a systematic prognostic review.
Literature search
The study period was the last 20 years (2000-2020) and the search period was between August 1 and August 30, 2020. The source of information was the scientific articles included in the review, therefore, the inclusion criteria were the scientific articles that address the influence of body mass index in pregnant women and its perinatal effects, scientific articles with observational, descriptive, cross-sectional methodological design, analytical cohort, and case-control studies, scientific articles with good methodological quality fulfilling the items of the tool STROBE and PRISMA. On the other hand, the exclusion criteria were specific studies that could not be applied in the areas of health, duplicate studies, and studies published outside the desired period and search period.
Frame 1
DeSC and MeSH descriptors used
|
Variables PICO |
Result of DeSC descriptors |
MeSH Descriptor Results |
|
Pregnant |
Pregnant woman |
Pregnant Women |
|
INC |
“Body mass index” |
Body Mass Index |
|
Perinatal effects |
“Perinatal mortality” / “Newborn” |
Infant Mortality Newborn |
The bibliographic search strategies were carried out through four steps: a) the identification of the search terms (thesauri), through the use of DeSC (descriptors of health science) where the PICO variables were introduced for the identification of the thesauri that were used in the search process; b) checking the similarities of the DeSC and MeSH descriptors, verifying the number of the identifying IDs in both (see table); (c) the construction and definition of the search string, using the logical or boolean (DNA) operative; d) and the application of search strategies, where for this systematic review, the specific MeSH descriptors were used for the search that, in the first instance, was carried out independently for each of the MeSH terms and then with them combined (Table 1).
The limits or filters established for the search strategy were the following: Studies carried out in humans, female sex, and adult patients, Publications in English and Spanish, Published in the last 20 years, where 200 articles were identified through the use of the PRISMA diagram included a total of 9 scientific articles for this review. (Figure 1).
Figure 1
PRISMA flowchart: Search strategy, selection process, and exclusion of studies included in this systematic review
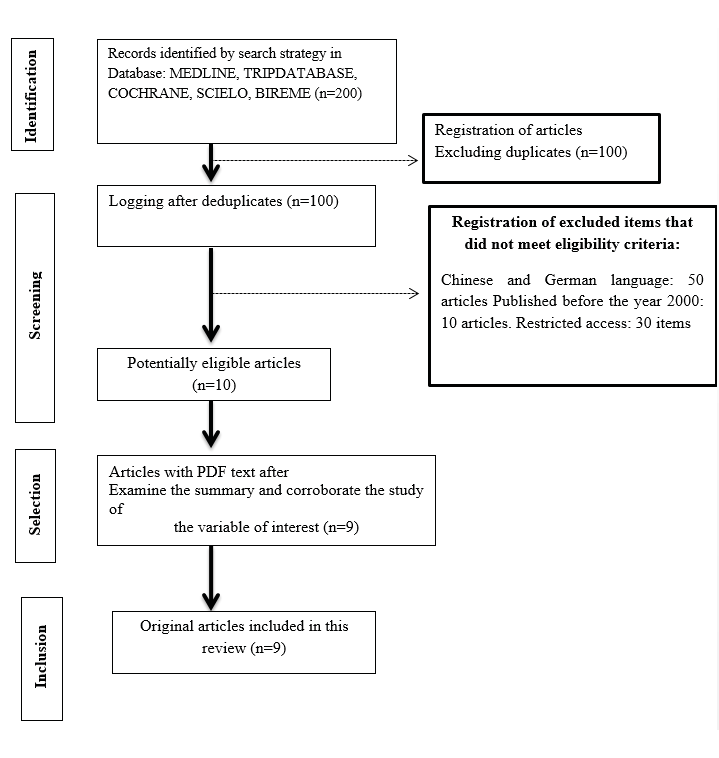
Source: Adapted from the guide of methodological aspects to be evaluated in a systematic review, UNICA (2020).
RESULTS AND DISCUSSION: SUMMARY OF EVIDENCE:
The articles taken for this review showed differences in certain concepts, constructs, objectives, and methods used. To give homogeneity to the evidence presented, the studies were grouped into sections related to the main variables studied, in terms of perinatal outcomes associated with altered BMI in pregnant women. The sections used to summarize the perinatal outcomes associated with altered BMI in pregnant women were: overweight, obese, and underweight women during pregnancy, as they are at risk of being large for gestational age newborn, emergency cesarean delivery, labor induction number, and fetal macrosomia (>4,250 grams). The only maternal risk factor reported and associated with overweight and obesity was the risk of Hypertension and Gestational Diabetes.
Because of the purpose of this review, the description of the results of the articles included in each section includes the most outstanding methodological aspects, as well as the main findings of the studies, exclusively about perinatal outcomes concerning altered BMI in pregnant women (Table 1).
Table 1
Table-summary of the results of the bibliographic search
|
Publication data |
|||||
|
Item Number (ID) |
Authors and year of publication |
Type of Publication |
Country of publication |
Language of publication |
Posted on |
|
1 |
Ehrenberg et al. (2004) |
Original article |
United States |
English |
American Journal of Obstetrics and Gynecology, 191 (3), 964-968 |
|
2 |
Zhao et al. (2017) |
Original article |
China |
Chinese-English |
Chinese Journal of Obstetrics and Gynecology, 52 (11): 757 -764 |
|
3 |
Goldstein et al. (2017) |
Original article |
United States |
English |
JAMA, 317 (21), 2207-2225 |
|
4 |
Durst et al. (2016) |
Original article |
United States |
English |
American Journal of Perinatology, 33 (9), 849-855 |
|
5 |
Kominiarek et al. (2015) |
Original article |
United States |
English |
Obstetrics Gynecol. October 2018; 132 (4): 875-881. |
|
6 |
Hung et al. (2015) |
Original article |
China |
Chinese-English |
Taiwanese Journal of Obstetrics & Gynecology, 54(4), 421–425. |
|
7 |
Wen & Lv, (2015) |
Original article |
China |
Chinese-English |
International Journal of Clinical and experimental medicine, 8(2), 2881–2886. |
|
8 |
Cedergren, (2006) |
Original article |
Sweden |
English |
International journal of gynaecology and obstetrics: 93(3), 269–274 |
|
9 |
De la Calle et al. (2009) |
Original article |
Chile |
Spanish |
REV CHIL OBSTET GINECOL 2009; 74(4): 233 - 238 |
Some articles also included other study variables; These have not been collected because they do not constitute the objective of this work. It should be noted that the United States represented the country with the largest scientific publications related to the subject, it is said that this could be explained by the lifestyle of the American population since this country has a high rate of obesity in its population and that is why the concern of the health system to investigate this association, is due to the above. The year 2015 and 2017 with 22.2% (n=2) respectively, were the years in which the most frequently published research addressing the relationship between maternal BMI and perinatal effects, followed by 2004, 2006, 2009, 2016, 2018, with 11.1% (n=1) respectively (Table 1.1).
55.5% (n=5) of the articles were published in English, followed by English-Chinese with 33.3% (n=3), and in third place Spanish with 11.1% (n=1). The language of scientific publication disclosed in the journals is the English language, in our review it accounted for 56% of the articles (five articles) included in this review, so we reiterate the importance for health personnel to know and understand the English language to keep up with new medical advances.
Table 1.1
Table-summary of the results of the bibliographic search
|
Contents of the publication |
|||||||
|
ID |
Research Design |
Period, sample |
Variables studied |
Main results |
Conclusions of the Study |
Methodological Quality |
Quality of the evidence (GRADE) |
|
1 |
Not described (it is implicitly described in the material and method section) being the type of study Cohort) |
1997 to June 2001 12,950 deliveries |
BMI Classification Perinatal outcomes |
BMI classification according to WHO: Overweight: 23.7% (n=2,991) Underweight: 13.0% (n= 1,640) Obese: 23.2% (n=2,928) Perinatal outcomes: Obese women had an elevated risk of large-for-gestational-age delivery (16.8% vs. 10.5%; P <0.0001) as well as overweight women (12.3% vs. 10.5%; P = 0.01). |
Pregestational obesity is independently associated with an increased risk of large-for-gestational-age delivery. |
STROBE 21 |
Moderate |
|
2 |
Cohort |
1/ 08/2014- 30/ 09/2015 6 908 pregnant women |
BMI Classification Perinatal outcomes |
BMI classification according to WHO: Low weight: 17.39%, (n=1201) Normal weight: 73.00% (n=5 04) Overweight and obesity: 9.61% (n=664) Perinatal outcomes: Overweight and obesity were associated with an increased risk of nulliparous emergency cesarean section, with the OR of 1.66 95% CI: 1.27-2.16 Underweight was associated with a lower [risk of emergency cesarean section With OR = 0.66, ] [95% CI 0.48 to 0.90] |
Overweight and obese women have an increased risk of emergency cesarean section. |
STROBE 22 |
Moderate |
|
3 |
Systematic review |
January 1, 1999, and February 7, 2017 |
Weight gain (IOM) Perinatal outcomes |
Below-recommended gestational weight gain (MIO) was associated: Increased risk of small-for-gestational-age (OR, 1.53 [95% CI, 1.44-1.64]. Increased risk for acute respiratory disease 5% [95% CI, 4%-6%]). Increased risk of preterm birth (OR, 1.70 [1.32-2.20]; Lower risk of Large-for-gestational age (OR, 0.59 [0.55-0.64]; Lower risk of macrosomia (OR, 0.60 [0.52-0.68]; cesarean delivery showed no significant difference (OR, 0.98 [0.96-1.02]; Gestational weight gain above recommendations was associated with Lower risk of Small for gestational age (OR, 0.66 [0.63-0.69]; Lower risk of preterm birth (OR, 0.77 [0.69-0.86 Higher risk of Grade for gestational age (OR, 1.85 [1.76-1.95]; Increased risk of macrosomia (OR, 1.95 [1.79-2.11]; cesarean delivery (OR, 1.30 [1.25-1.35]) |
Gestational weight gain greater or less than guideline recommendations, compared with weight gain within recommended levels, was associated with an increased risk of adverse maternal and infant outcomes. |
PRISMA 27 |
HIGH |
|
4 |
Retrospective cohort |
1 January-December 2009 5,651 obese women |
Gestational weight gain (GWG) in obese women Perinatal outcomes |
Gestational weight gain above recommendations was associated with increased risk: Caesarean section (OR: 1.44, 95% CI: 1.21-1.72), Gestational hypertension (OR: 1.58, 95% CI: 1.21-2.06) Macrosomia (birth weight ≥ 4,250 g) (OR: 2.08, 95% CI: 1.62-2.67). Below recommendations gestational weight gain (IOM) was associated: Small for gestational age infants (OR: 0.60, 95% CI: 0.47-0.75). Minimum weekly gestational weight gain of recommendations (OR) was associated: with spontaneous preterm birth (OR: 1.56, 95% CI: 1.23-1.98) and smaller for infants of gestational age (OR: 1.55, 95% CI: 1.19-2.01). Excessive weekly gestational weight gain of recommendations (IOM) was associated: with indicated preterm delivery (OR: 1.61, 95% CI: 1.29-2.01), cesarean section (OR: 1.39, 95% CI: 1.20-1.61), Preeclampsia (OR: 1, 83, 95% CI: 1.49-2.26). Neonatal intensive care unit admission (OR: 1.33, 95% CI: 1.08-1.63) Macrosomia (OR: 2.40, 95% CI: 1.94-2.96). |
Obese women with excessive GWG had worse outcomes than women with GWG within the recommendations. Limited GWG was associated with an increase in spontaneous preterm births and SGA infants. |
STROBE 22 |
Moderate |
|
5 |
Retrospective cohort |
2008-2011 29,861 women |
Gestational weight gain Perinatal outcomes |
Maternal Outcomes: Gestational weight gain above IOM guidelines was associated with the risk of Cesarean delivery in nulliparous women (OR: 1.44, 95% CI 1.31-1.59) and multiparous women (OR: 1.26, 95% CI 1.13-1.41) Hypertensive diseases of pregnancy in nulliparous and multiparous women ( OR: 1.84; CI95%: 1.66-2.04). For neonatal outcomes: Gestational weight gain above IOM guidelines is shoulder dystocia (OR: 1.74, CI: 95% 1.41-2.14), Macrosomia (OR: 2.66, 95% CI 2.03-3.48 ) Neonatal hypoglycemia (OR: 1.60, 95% CI 1.16-2.22). Gestational weight gain below IOM guidelines Spontaneous preterm delivery (OR: 1.50, 95%CI 1.31-1.) |
Gestational weight gain below or above guidelines is associated with a variety of adverse pregnancy outcomes. |
STROBE 22 |
Moderate |
|
6 |
Retrospective cohort |
2009 and 2014 9301 pregnancies |
Increased gestational weight Perinatal outcomes |
Gestational weight gain above IOM guidelines was associated with a risk of Preeclampsia [OR: 3.0 95% CI 1.9-4.7], Primary cesarean delivery (OR: 1.4, 95% CI 1.2-1.6) due to dysfunctional labor and cephalopelvic disproportion. Large for gestational age (OR: 1.8; CI 95%: 1.5-2.1) Macrosomic newborns (OR: 2, 2; CI 95%: 1.6-3.1). Gestational weight gain below IOM guidelines was associated with the risk of: Diagnosed with gestational diabetes mellitus (OR 1.5, CI: 95% 1.3-1.8) Placental abruption (OR: 1.7, 95% CI 1.1-2.5), Small-for-gestational age infants (OR: 1.6; CI 95%: 1.4-1.9) Low birth weight infants (OR 1.9; CI95%: 1.4–2.4) |
Women with gestational weight gain outside the 2009 IOM guidelines were at risk for adverse maternal and neonatal outcomes. |
STROBE 22 |
Moderate |
|
7 |
Retrospective cohort |
2009-2013 13776 women |
Gestational weight gain Neonatal outcomes |
For neonatal outcomes: Inadequate gestational weight gain according to IOM guidelines the Higher risk of LBW (OR: 2.13, 95% CI: 1.75, 2.86) Preterm birth (OR: 1.44, 95% CI: 1.21, 1.67) than those in the adequate gestational weight gain group, Not associated with longer hospital stay (OR: 1.13, 95% CI: 0.91-1.43) In addition, the rate of birth asphyxia and NICU admission were similar in both groups (P> 0.05). |
Normal-weight pregnant women with GWG below the guidelines recommended by IOM 2009 were found to have an increased risk of low birth weight and preterm birth. |
STROBE 22 |
Moderate |
|
8 |
Systematic review + meta-analysis |
2014 42 studies |
Gestational weight gain Perinatal outcomes |
Maternal Outcomes: Gestational weight gain below IOM guidelines was associated with a lower risk of: Preeclampsia (OR: 0.52; CI95: 42- 0.62), Caesarean section (OR: 0.81; CI95: 0.73-0.90), instrumental delivery (OR: 0.75; CI95: 0.63-0.88) Large for gestational age (OR: 0.66; CI95: 0.59-0.75). There was a 2-fold increased risk of preeclampsia and large-for-gestational-age babies among average, overweight women with excessive weight gain. High gestational weight gain increased the risk of cesarean delivery in all maternal BMI classes. |
The effects of high or low gestational weight gain differ depending on maternal BMI and the outcome variable studied. Obese women may benefit from low weight gain during pregnancy. |
PRISMA 27 |
HIGH |
|
9 |
Transverse |
2007-2008 1,223 pregnant women |
INC Neonatal outcomes |
Overweight pregnant women have Three times the increased risk of cesarean section OR: 1.9; CI95% 1.4-2.5) Number of labor induction (OR: 1.7; CI95% 1.4-1.9) fetal macrosomia (>4,000 grams) (OR: 1.5; CI95% 1.4-2.2) Pregnant women with obese women have: Three times cesarean section risk (OR: 3.1; CI95% 2.8-4.3). The number of labor inductions (OR: 2.0; CI 95% 1.8-2.9). fetal macrosomia (>4,000 grams) (OR: 1.9; CI95% 1.3-2.8) In the multivariate logistic regression analysis (adjusting for age, diabetes, and gestational hypertension) the association between overweight and cesarean section persisted (OR: 2.1; CI95% 1.7-2.7) and between obesity and cesarean section (OR: 3.0; CI95% 2.6-3.8). |
Maternal overweight and obesity in early pregnancy are associated with an increase in the number of cesarean sections and inductions of labor |
STROBE 22 |
Moderate |
55.5% (n=5) of the articles were published in English (Table 1). The language of scientific publication published in the journals is the English language, in this review, it accounted for 56% of the articles (five articles) included, so we reiterate the importance for health personnel to know and understand the English language to keep up with new medical advances. Three out of nine scientific articles were found, which took into account the alteration of the body mass index and its classification according to the WHO and the perinatal effects that this brings. Tables 1 and 1.1 show that only one article, which was conducted by Zhao et al (2017) studied the association of low maternal weight and perinatal effects, finding that this represents a lower risk for emergency cesarean delivery in underweight pregnant women, compared to the risk reported for overweight and obese pregnant women.
Tabla 2
Perinatal results found in scientific articles
|
(ID) |
Authors |
Year of publication |
Perinatal results according to BMI alteration and its classification according to WHO |
Perinatal Results According to Weight Gain Gestational according to IOM recommendations |
|
1 |
Ehrenberg et al. |
2004 |
Obese women OR: 16.8% of the delivery grade for gestational age Overweight women OR: 10.5% of the delivery grade for gestational age |
Not reported |
|
2 |
Zhao et al. |
2017 |
Overweight and obese women OR: 1.66 cesarean delivery of Emergency in nulliparous patients. Underweight woman Emergency cesarean section OR:0.66 |
Not reported |
|
3 |
Goldstein et al. |
2017 |
Not reported |
Gestational weight gain below recommendations (IOM) risk of: • Small for gestational age OR: 1.53 • Acute respiratory disease OR: 5 • Premature birth OR: 1.70 • Cesarean delivery OR: 1.30 • Large for gestational age OR:0.59, • Macrosomía OR, 0,60 • Cesarean delivery showed no significant difference Gestational weight gain above IOM recommendations was associated with: • Small for gestational age OR. 0,66 • Premature birth OR: 0.77 • Large for gestational age OR:1.85 • Macrosomía OR:1,95 |
|
4 |
Durst et al. |
2016 |
Not reported |
Gestational weight gain above recommendations (IOM) was associated with risk: • Cesarean section OR: 1.44. • Gestational hypertension OR: 1.58. • Macrosomia (birth weight ≥ 4,250 g) OR: 2.08. Gestational weight gain below recommendations (IOM) were associated: • Small for gestational age OR: 0.60. Minimum weekly gestational weight gain of recommendations (IOM) was associated: • Spontaneous preterm birth OR: 1.56. • Small for gestational age OR: 1.55 Weekly Excessive Gestational Weight Gain (IOM) was associated: • Preterm birth indicated OR: 1.61 • Cesarean section OR: 1.39 • Preeclampsia OR: 1, 83 • NICU admission OR: 1.33 • Macrosomía OR: 2,40 |
|
5 |
Kominiarek et al. |
2018 |
Not reported |
Gestational weight gain above IOM guidelines was associated with the risk of: • Cesarean delivery in nulliparous women OR: 1.44 and multiparous OR: 1.26. • Hypertensive diseases of pregnancy in nulliparous and multiparous women OR: 1.84 • Shoulder dystocia OR:1.74 Macrosomia OR: 2.66 Gestational weight gain below IOM guidelines • Spontaneous preterm birth OR: 1.50 • Hipoglucemia neonatal OR: 1,60 |
|
6 |
Hung et al. |
2015 |
Gestational weight gain above IOM guidelines was associated with the risk of: • Preeclampsia OR: 3,0 • Cesarean delivery due to dysfunctional labor and cephalopelvic disproportion. OR:1,4 • Large for gestational age OR:1,8 • Macrosómicos OR: 2,2 Gestational weight gain below IOM guidelines was associated with the risk of: • Diagnosed with gestational diabetes mellitus OR:1,5 • Placental abruption OR:1,7 • Small-for-gestational-age infants OR:1,6 • Low birth weight infants OR: 1.9 |
|
|
7 |
Wen and Lv |
2015 |
Not reported |
Inadequate gestational weight gain according to IOM guidelines: • BPN OR: 2,13. • Preterm birth OR:1.44, than those in the adequate gestational weight gain group, • Not associated with longer hospital stay OR: 1.13 • In addition, the birth asphyxia rate and NICU admission were similar in both groups (P> 0.05). |
|
8 |
Cedergren |
2006 |
Not reported |
Gestational weight gain below IOM guidelines was associated with a lower risk of: • Preeclampsia OR:0,52 • Cesarean section OR:0.81 • Parto instrumental OR: 0,75 • Large for gestational age OR: 0.66 |
|
9 |
De la Calle et al. |
2009 |
Overweight pregnant women: • Cesarean section OR: 1.9 • Number of labor induction OR: 1,7 • Macrosomía fetal (>4.250 gramos) OR: 1,5 Pregnant women with obesity: • Cesáreas OR: 3,1 • Number of labor inductions OR: 2.0 • Macrosomía fetal (>4.250 gramos) OR: 1,9 • Gestational Hypertension and Diabetes Mellitus in patients with overweight and obesity OR: 3.0 |
Not reported |
Note: ID: Identification of the item, which corresponds to the number assigned to the item during the selection process.
Source: Articles included in this review.
In the three articles that reported more neonatal than fetal risk factors (Table 2.1), it was reported that the following neonatal risk factors associated with obesity and overweight are: large for gestational age newborn, emergency cesarean delivery, labor induction number, and fetal macrosomia (>4,250 grams). The only maternal risk factor reported and associated with overweight and obesity was the risk of hypertension and gestational diabetes. The fact that most studies reported the perinatal effect of obesity and maternal overweight may be closely related to the fact that, in daily clinical practice, it is more evident to observe overweight or obese patients than underweight.
Table 2.1
Perinatal outcomes according to Alteration of maternal BMI during gestation identified in the included articles
|
ID |
Perinatal results according to alteration of maternal BMI during pregnancy |
Low weight |
Overweight |
Obesity |
|
Risk |
Risk |
Risk |
||
|
1 |
Large-for-gestational-age delivery |
Not calculated |
OR:10,5 |
OR:16,8 |
|
2 |
Emergency cesarean delivery |
OR:0,66 |
OR: 1,66 |
OR: 1,66 |
|
Not calculated |
OR:1,9 |
OR:3,1 |
||
|
9 |
Labor induction number |
Not calculated |
OR:1,7 |
OR:2,0 |
|
Fetal macrosomia (>4,250 grams) |
Not calculated |
OR:1,5 |
OR:1,9 |
|
|
Hypertension and Gestational Diabetes |
Not calculated |
OR:3,0 |
OR:3,0 |
Note: OR: Obbs Ratio, also known as odds ratio, is a risk measure used to express a causal association between two or more variables, It is considered a risk factor if the OR is greater than one if it is less than one it is considered a protective factor.
Source: Articles included in this review.
Table 2.2.
Perinatal results according to Gestational Weight Gain according to IOM recommendations during gestation identified in the included articles
|
ID |
Perinatal outcomes according to Gestational Weight Gain according to IOM recommendations |
Gestational weight gain below |
Minimal gestational weight gain |
Gestational weight gain above - Excessive |
|
Risk |
Risk |
Risk |
||
|
8 |
Large-for-gestational-age newborn |
OR:0,66 |
Not calculated |
Not calculated |
|
Preeclampsia |
OR:0,52 |
Not calculated |
Not calculated |
|
|
Emergency cesarean delivery |
OR:0,81 |
Not calculated |
Not calculated |
|
|
Instrumental childbirth |
OR: 0,75 |
Not calculated |
Not calculated |
|
|
7 |
Low birth weight |
OR: 2,13. |
Not calculated |
Not calculated |
|
Premature |
OR:1,44 |
Not calculated |
Not calculated |
|
|
Longer hospital stay |
OR: 1,13 |
Not calculated |
Not calculated |
|
|
Birth asphyxia and NICU admission |
Not calculated |
Not calculated |
Not calculated |
|
|
6 |
Gestational Diabetes |
OR:1,5 |
Not calculated |
Not calculated |
|
Preeclampsia |
Not calculated |
Not calculated |
OR: 3,0 |
|
|
Placental abruption |
OR:1,7 |
Not calculated |
Not calculated |
|
|
Cesarean delivery due to dysfunctional labor and cephalopelvic disproportion |
Not calculated |
Not calculated |
OR:1,4 |
|
|
Large for gestational age |
Not calculated |
Not calculated |
OR:1,8 |
|
|
Macrosomía |
Not calculated |
Not calculated |
OR: 2,2 |
|
|
Small-for-gestational-age newborns |
OR:1,6 |
Not calculated |
Not calculated |
|
|
Small newborn at birth |
OR: 1,9 |
Not calculated |
Not calculated |
|
|
5 |
Spontaneous preterm birth |
OR: 1,50 |
Not calculated |
Not calculated |
|
Neonatal hypoglycemia |
OR: 1,60 |
Not calculated |
Not calculated |
|
|
Macrosomía |
Not calculated |
Not calculated |
OR: 2,66 |
|
|
Shoulder Dystocia |
Not calculated |
Not calculated |
OR:1,74 |
|
|
Hypertensive disease of pregnancy |
Not calculated |
Not calculated |
OR: 1,84 |
|
|
Cesarean Delivery |
Not calculated |
Not calculated |
OR:1,26 |
|
|
4 |
Cesarean Delivery |
Not calculated |
Not calculated |
OR: 1,44 -OR: 1,39 |
|
Gestational hypertension |
Not calculated |
Not calculated |
OR: 1,58. |
|
|
Macrosomía |
Not calculated |
Not calculated |
OR: 2,08 - OR:2,40 |
|
|
Newborns small for at gestational age. |
OR: 0,60 |
OR: 1,55 |
OR: 2,40 |
|
|
Spontaneous preterm birth |
Not calculated |
Not calculated |
OR: 1,61 |
|
|
Preeclampsia |
Not calculated |
Not calculated |
OR: 1, 83 |
|
|
NICU Admission |
Not calculated |
Not calculated |
OR: 1,33 |
|
|
3 |
Macrosomía |
OR, 0,60 |
Not calculated |
OR:1,95 |
|
Acute respiratory illness |
OR:5 |
Not calculated |
Not calculated |
|
|
Small-for-gestational-age newborns |
OR: 1,53 |
Not calculated |
OR. 0,66 |
|
|
Large-for-gestational-age newborns |
OR:0,59 |
Not calculated |
OR:1,85 |
|
|
Premature |
OR: 1,70 |
Not calculated |
OR: 0,77 |
|
|
Cesarean Delivery |
No significant differences |
No significant differences |
OR: 1,30 |
Note: OR: Obbs Ratio, also known as odds ratio, is a risk measure used to express a causal association between two or more variables, It is considered a risk factor if the OR is greater than one if it is less than one it is considered a protective factor.
Source: Articles included in this review.
Gestational weight gain above what is recommended according to IOM guidelines was a risk factor for cesarean section in four of the five articles in which this relationship was studied. The risk of hypertensive disease of pregnancy (Preeclampsia, Gestational hypertension) was three times higher compared to the 38 pregnant women who presented a minimal or lower increase than recommended, the risk of Fetal Macrosomia was two to three times higher in pregnant women with an excessive increase, compared to pregnant women with minimal increase. Excessive weight gain as recommended by the IOM guidelines was also a risk factor for Shoulder Dystocia and NICU admission, it is worth mentioning that it was a protective factor for preterm birth and small for gestational age newborns.
Pregnancy weight gain below the recommended IOM guidelines was a risk factor for preterm birth in three of the four articles where this association was reported. Newborn small for gestational age, reported in three articles of which one reported to be a protective factor with an OR 0.6. Acute respiratory disease reported in an article with an OR: 5, was not a protective factor for newborns large for gestational age, instrumental delivery, the risk of cesarean section, was not significant concerning minimal or excessive weight gain, gestational weight gain below recommended also posed a risk factor for low birth weight, placental abruption, gestational diabetes. The increase in gestational weight below that recommended according to the IOM guidelines was a protective factor for fetal macrosomia identified in three articles and reported only in one article with an OR: 0.60, hypertensive disorders (preeclampsia, gestational hypertension) was a protective factor in four of the articles. (Table 2.2)
On the other hand, the minimum gestational weight gain recommended according to the IOM guidelines was a risk factor for Small Gestational Age Newborns (SGA) with an OR: 1.55, it was identified that cesarean delivery did not present significant differences when compared with pregnant women who presented a weight gain below the recommended. It is worth mentioning that the minimum gestational weight gain was not studied in seven articles of the nine, possibly this is because the impact it has on the clinical outcome of pregnancy presents certain similarities with weight gain below that recommended by the IOM. (Table 2.2)
CONCLUSION AND RECOMMENDATIONS (GRADE)
As a conclusion of this systematic review article, we identified the relationship between body mass index before and during pregnancy with the perinatal effects that the baby or mother in question may have. Mothers who were overweight or obese had a higher association of hypertensive disorders (pre-eclampsia, gestational hypertension), having a large-for-gestational-age baby (macrosomia), increased chances of emergency cesarean delivery, or having gestational diabetes. It should be noted that, although pregnant women have minimal or below IOM recommendations, they will have a higher risk of premature birth, newborn babies small for gestational age, acute respiratory diseases, low birth weight (LBW), placental abruption, gestational diabetes, and neonatal hypoglycemia.
DECLARATION OF INTERESTS
Conflict of interest
The authors have declared that they have no conflict of interest, Source of funding: none.
Ethical approval
No ethical approval was required as this is a secondary analysis of data derived from published primary studies.
AUTHORS’ CONTRIBUTION
Renaldy ESPINOZA-SOTELO preparation first and latest version of the article, data extraction, searching, study identification.
Alexis, AGUILAR-MEZA: protocol development and research report, data extraction, searches, study identification.
Fernanda PINEDA-GEA: evaluation of the quality of data extraction, searches, study identification, data extraction, and preparation of the first and last version of the manuscript for review.
René GUTIERRÉZ-ABURTO: preparation of the manuscript for review.
All authors have reviewed and approved the final version of the text.
Work cited
Cedergren M. (2006). Effects of gestational weight gain and body mass index on obstetric outcome in Sweden. International Journal of Gynecology and Obstetrics, 93(3), 269–274. https://doi.org/10.1016/j.ijgo.2006.03.002
Cedergren M. I. (2004). Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstetrics and Gynecology, 103(2), 219–224. https://doi.org/10.1097/01.AOG.0000107291.46159.00
De la Calle FM, M., Armijo, O., Martín, E., Sancha, M., Magdaleno, F., Omeñaca, F. and González G, A. (2009). OVERWEIGHT AND PREGESTATIONAL OBESITY AS A RISK FACTOR FOR CESAREAN SECTION AND PERINATAL COMPLICATIONS. Revista chilena de obstetricia y ginecología, 74(4), 233-238. https://dx.doi.org/10.4067/S0717-75262009000400005
De la Plata Daza, M., Pantoja Garrido, M., Frias Sánchez, Z., & Rojo Novo, S., (2018). Influence of pregestational body mass index and maternal weight gain on maternal-fetal perinatal outcomes. Cuban Magazine of
De León- Gálvez., F., Delgado, H., (2016). Maternal body mass index and newborn weight. Rev. Fac. Med, Vol. 1 2016, Jul–Dec No. 21. https://docs.bvsalud.org/biblioref/2019/01/969493/indice-de-masa-corporal-materno-y-peso-del-recien-nacido.pdf
Durst, J. K., Sutton, A. L., Cliver, S. P., Tita, A. T., & Biggio, J. R. (2016). Impact of gestational weight gain on perinatal outcomes in obese women. American Journal of Perinatology, 33(9), 849–855. https://doi.org/10.1055/s-0036-1579650
Ehrenberg, H. M., Mercer, B. M., & Catalano, P. M. (2004). The influence of obesity and diabetes on the prevalence of macrosomia. American Journal of Gynecology and Obstetrics, 191(3), 964–968. https://doi.org/10.1016/j.ajog.2004.05.052
Gilmore, LA and Redman, LM. (2015). Weight Gain During Pregnancy and Implementation of the 2009 IOM Guidelines: Towards a Uniform Approach. Obesity (Silver Spring, Maryland), 23(3), 507–511 https://doi.org/10.1002/oby.20951
Goldstein, R. F., Abell, S. K., Ranasinha, S., Misso, M., Boyle, J. A., Black, M. H., Li, N., Hu, G., Corrado, F., Rode, L., Kim, Y. J., Haugen, M., Song, W. O., Kim, M. H., Bogaerts, A., Devlieger, R., Chung, J. H., & Teede, H. J. (2017). Association of gestational weight gain with maternal and infant outcomes: A systematic review and meta-analysis. JAMA, 317(21), 2207–2225. https://doi.org/10.1001/jama.2017.3635
Hung, T. H., Chen, S. F., Hsu, J. J., & Hsieh, T. T. (2015). Gestational weight gain and risks of adverse perinatal outcomes: a retrospective cohort study based on 2009 Institute of Medicine guidelines. Taiwanese Journal of Obstetrics and Gynecology, 54(4), 421–425. https://doi.org/10.1016/j.tjog.2015.06.010
IOM (Institute of Medicine). 2009. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington, DC: The National Academies Press. https://www.cbsnews.com/htdocs/pdf/052809_pregnancy.pdf
Kominiarek, M. A., Saade, G., Mele, L., Bailit, J., Reddy, U. M., Wapner, R. J., Varner, M. W., Thorp, J. M., Jr, Caritis, S. N., Prasad, M., Tita, A., Sorokin, Y., Rouse, D. J., Blackwell, S. C., Tolosa, J. E., y Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units (MFMU) Network (2018). Asociación entre la ganancia de pesos gestacional y los resultados perinatales. Obstetricia y Ginecología, 132(4), 875–881. https://doi.org/10.1097/AOG.0000000000002854
Maldonado-Durán M, Sauceda-García JM., and Lartigue T. (2008). Physiological and emotional changes during normal pregnancy and fetal behavior. Perinatol Reprod Hum, 22(1), 5-14. https://www.medigraphic.com/cgi-bin/new/resumenI.cgi?IDARTICULO=21076
Minjarez-Corral, M., Rincón-Gómez, I., Morales-Chomina, Y., Espinosa-Velasco, M., Zárate, A., & Hernández-Valencia, M. (2014). Gestational weight gain is a risk factor for developing obstetric complications. Perinatology and Human Reproduction, 28(3), 159-166. http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0187-53372014000300007&lng=es&tlng=es.
Obstetrics and Gynecology, 44(1), 1-9. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0138-600X2018000100007&lng=es&tlng=es
Ramos-Hernández, A., Martínez-Nuñez, L., León-López, A., Hoyos-Garza, A., & Zavala-García, A. (2021). Perinatal outcomes in women according to BMI: a multicenter study of public and private hospitals. Revista del Hospital Juárez de México, 88(2), 56-62. https://web.archive.org/web/20210716143420id_/https://www.revistahospitaljuarez.com/files/rhjm_21_88_2_056-062.pdf
STROBE. (2009). STROBE verification tool. Retrieved November 4, 2020, https://www.strobe-statement.org/index.php?id=available-checklists
Wen, T., & Lv, Y. (2015). Inadequate gestational weight gain and adverse pregnancy outcomes among normal-weight women in China. International Journal of Clinical and Experimental Medicine, 8(2), 2881–2886. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4402896/
Zhao, R. F., Zhang, W. Y., & Zhou, L. (2017). Relationship between the risk of emergency cesarean section by nulliparous section with body mass index before pregnancy or gestational weight gain. Chinese Journal of Obstetrics and Gynecology, 52(11):757-764. https://doi.org/10.3760/cma.j.issn.0529-567X.2017.11.008
