ISSN 2410-5708 / e-ISSN 2313-7215
Year 13 | No. 37 | June - September 2024
© Copyright (2024). National Autonomous University of Nicaragua, Managua.
This document is under a Creative Commons
Attribution-NonCommercial-NoDerivs 4.0 International licence.
Meckel's diverticulum in Nicaraguan adults. Report of two cases and review of the literature.
https://doi.org/10.5377/rtu.v13i38.19125
Submitted on february 5th, 2024 / Accepted on august 26th, 2024
José Arnoldo González Bermúdez
General practitioner. A resident of the specialty in General Surgery.
Hospital Alemán Nicaragüense, Managua, Nicaragua.
Fernanda Pineda Gea
General practitioner. Hearing prosthetist, Master in Education, Teaching and University Research, USMP, Peru.
University Professor at Universidad Católica Redemptoris Mater Managua, Nicaragua
Section: Health and Social Services
Scientific research article
Keywords: University Professor at Universidad Católica Redemptoris Mater Managua, Nicaragua
Abstract
The cases described discuss the prevalence of this clinical entity simulating an acute surgical abdomen in adult men and compare the approach of symptomatic and asymptomatic Meckel’s diverticulum
Methods: This case report was reported using the international guidelines that guide the aspects of writing and publishing a surgical case report, mentioned in the SCARE guideline (Surgical Case Report, 2020)
Case presentation: Male patients aged 31 (case 1) and 19 years (case 2) respectively, who came to the unit with acute surgical abdomen in which Meckel’s diverticulum was diagnosed incidentally (case 1) concomitant with acute appendicitis and symptomatic (case 2) complicated by inflammation, a location was observed on the antimeenteric side of the ileum, more or less 80 cm concerning the ileocecal valve, with a length ranging from 2 (case 1) to 10 mm (case 2). Diverticulectomy was performed using the wedge reception technique with primary anastomosis (case 1) and intestinal reception with approximately 5cm margin of the diverticulum with end-to-end anastomosis in two planes (case 2). The approach was successful in both patients.
Conclusion: The diagnosis of complicated Meckel’s diverticulum in adults is difficult because the clinical characteristics in patients with complications are nonspecific and it is not clinically distinguished from appendicitis, exploratory laparotomy seems to be an ideal surgical course in cases of acute surgical abdomen with an uncertain diagnosis.
INTRODUCTION AND IMPORTANCE
Meckel’s diverticulum is the most common congenital anomaly of the gastrointestinal tract and occurs in 2% of the population (Shirakabe & Mizokami, 2023). The characteristics of Meckel’s diverticulum, according to Murruste et al. (2014), can best be remembered by the “rule of two”: it occurs in 2% of the population; It is usually discovered before the age of 2; it is 2 inches long and 2 cm in diameter; it is located 2 feet proximal to the ileocecal valve; it is 2 times more common in men; and only 2% of individuals with Meckel’s diverticulum are symptomatic. The literature shows that it is more frequent in the pediatric age, so in the cases described the prevalence of this clinical entity simulating an acute surgical abdomen in adult men is discussed. In addition, the approach to symptomatic and asymptomatic Meckel’s diverticulum is compared.
METHODS
This case report was reported using the international guidelines that guide the aspects of writing and publishing surgical case reports, mentioned in the SCARE Guideline (Surgical Case Report, 2020) published by Agha et al. (2020). An observational, descriptive, prospective study was conducted. Data collection was carried out during the patient’s hospital stay in the General Surgery service of the German Nicaraguan Hospital.
CASE PRESENTATION
Case 1
A 31-year-old male patient, a mestizo, from the urban area of Managua, a university student, went to the emergency area of the hospital complaining of pain in the lower right quadrant with less than 24 hours of evolution and unquantified thermal rises. Pathological and non-pathological personal history, as well as surgical history, were denied. Physical examination revealed clear signs of acute abdomen with the presence of appendicular signs. Paraclinical examinations included a complete blood count at admission, which showed leukocytes 11820/uL, neutrophils 9621/uL, hematocrit 41.0%, hemoglobin 13.5 g/dL and platelets 151,000/uL, evidencing data of systemic inflammatory response with leukocytosis and neutrophilia. The general urine examination showed normal parameters, ruling out urinary tract infection and renal colic. The patient was evaluated in conjunction with a surgical specialist, and it was decided to urgently admit him to the operating room with a diagnosis of uncomplicated acute appendicitis. Compliance with prophylactic antibiotic therapy (Cefazolin one gram intravenously to be administered in the operating room during induction) was indicated.
Case 2
A 19-year-old male patient, mestizo, from the urban area of Managua, went to the emergency area of the hospital, complaining of pain in the mesogastrium that migrated to the right iliac fossa, associated with nausea and vomiting. Pathological, non-pathological, and surgical personal history denied. Physical examination showed clear signs of acute abdomen, with positive Markle, McBurney, Blumberg, and Rovsing’s signs. Complete blood count showed the following results: leukocytes 9730/uL, neutrophils 6558/uL, hematocrit 42.8%, hemoglobin 14.2 g/dL, platelets 313,000/uL. During his stay in the emergency area, the diagnosis of renal colic and urinary tract infection was ruled out. The patient was evaluated in conjunction with a doctor specializing in surgery, and it was decided to admit him urgently to the operating room with a diagnosis of complicated acute appendicitis. Compliance with prophylactic antibiotic therapy (Cefazolin one gram intravenously to be administered in the operating room during induction) is indicated.
Intervention
Case 1
The patient was prepared for emergency surgery in the operating room, with a presurgical diagnosis of uncomplicated acute appendicitis. The surgical intervention, classified as class II surgery, was performed on 02/20/23 by Surgeon Dr. Mejía (Basic Physician), with the first assistant Dr. Hernández (Third Year Resident), and the second assistant Dr. González (Second Year Resident). Regional anesthesia (0.5% heavy bupivacaine, 15 ml administered in the epidural space at the level of the lumbar region) and preoperative sedation (Midazolam, initial dose: 3ml intravenously and maintenance dose 3ml every hour) were administered by anesthesiologist Dr. Martínez, who performed the spinal block. The intervention lasted one hour and ten minutes [Start 2:30 p.m. - End 3:40 pm]. The patient, in the supine position, underwent an appendectomy by conventional means of a McBurney incision. The transoperative findings (Table 1) confirmed the preoperative diagnosis of acute appendicitis, corroborating that the disease was in the suppurating phase, which was the cause of the acute abdomen. Incidentally, a solitary Meckel’s diverticulum, located 80 cm from the ileocecal valve, measuring 2x2 cm, was found. No perforation, ulceration of the ileal mucosa, inflammatory reaction, or fibrous bands obstructing the intestinal lumen were observed (Figure 1). A diverticulectomy was performed using the wedge resection technique with primary anastomosis. Both specimens (vermiform appendix and Meckel’s diverticulum) were sent to the pathology department for histopathological analysis. The patient’s transoperative evolution occurred without any eventuality, ending the intervention successfully.
Table 1
Transoperative Findings
|
Anatomical structure |
Procedure and Transoperative Finding |
|
|
CASE 1 |
Vermiform Apéndice |
Impingement, ligation, and dissection of the vermiform appendix in the retrocecal position of approximately 12 cm (three times its normal size), fibrinopurulent exudate is observed throughout its extension. Obstruction of the appendicular lumen by two fecal stools located in the middle third. Approximately 20ml of the inflammatory fluid contained within the appendix is drained. |
|
CASE 2 |
Vermiform Apéndice |
Impingement, ligation, and dissection of the vermiform appendix in a retrocecal position of normal appearance and size, without inflammatory changes. |
Source: Data were obtained from the operative notes of the clinical records of the patients under study
Figure 1
Meckel’s diverticulum observed in case1
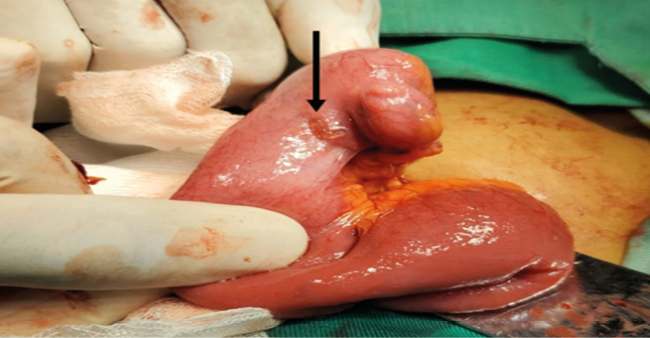
Note: The arrow in the figure shows Meckel’s diverticulum observed in the patient in case 1.
Source: Archive of images captured during operating room procedure
Case 2.
The patient was prepared for emergency surgery in the operating room, with a presurgical diagnosis of complicated acute appendicitis. The surgical intervention, classified as class II surgery, was performed on 10/02/23 by Surgeon Dr. Carmona (Basic Physician), with the first assistant Dr. Pérez (Third Year Resident), and the second assistant Dr. González (Second Year Resident). Regional anesthesia (0.5% heavy bupivacaine, 15ml administered in the epidural space at the level of the lumbar region) and preoperative sedation (Midazolam, initial dose: 3 ml intravenously and maintenance dose 5ml every hour) were administered by the anesthesiology specialist Dr. Mejía, who performed the spinal block. The intervention lasted two hours and thirty minutes [Start 1:57 pm - End 4:20 pm]. The patient, in the supine position, underwent a conventional appendectomy through a medium incision. The transoperative findings (Table 1) ruled out the preoperative diagnosis of complicated acute appendicitis, confirming that the appendix did not present inflammatory signs. The intestinal loops were inspected, and a solitary Meckel’s diverticulum, located 80 cm from the ileocecal valve, measuring 10x5 cm, was found. No perforation or ulceration was observed in the mucosa of the ileus, nor fibrous bands obstructing the intestinal lumen, although an inflammatory reaction was evident (Figure 2). A diverticulectomy was performed using the intestinal resection technique, with approximately 5 cm of diverticulum margin, and a two-plane end-to-end anastomosis. Both specimens (vermiform appendix and Meckel’s diverticulum) were sent to the pathology department for histopathological analysis. The patient’s transoperative evolution occurred without any eventuality, ending the intervention successfully.
The procedure carried out in the operating room
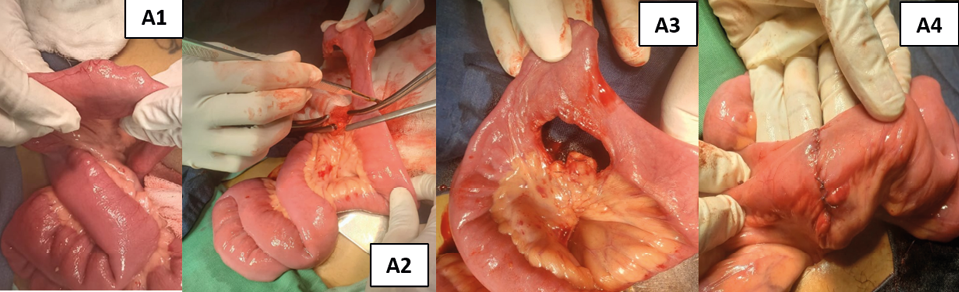
Source: Archive of images captured during operating room procedure
Postoperative evolution, follow-up
Both patients evolved satisfactorily in the general surgery room, continuing with medical management. Post-surgical paraclinical examinations showed clinical improvement; they did not present anemia or any evidence suggestive of infection. Intestinal transit and oral transit were restored after 24 hours. On the third post-surgical day, it was decided to discharge them from the hospital and the procedures were carried out to follow up with the surgeon in the hospital’s outpatient clinic. Biopsy results reported by the pathology department confirmed the diagnosis of diverticulitis.
DISCUSSION AND REVIEW OF THE LITERATURE
Epidemiological data
The epidemiological profile reported in the literature on Meckel’s diverticulum mentions a prevalence between 0.3% and 2.9% in the general population (Hansen & Søreide, 2018). This shows that the clinical presentation of this entity is rare. The fact that two cases have been diagnosed in the same year in the Nicaraguan population, where it had not been previously described, demonstrates the great theoretical contribution it represents to the Central American medical literature and especially for the scientific evidence generated in Nicaragua.
Anatomical features
According to the synthesis of the research consulted by Hansen and Søreide (2018), Meckel’s diverticulum is located between 7 and 200 cm proximal to the ileocecal valve (mean 52.4 cm), with a length that varies from 0.4 to 11.0 cm (mean 3.05 cm) and a diameter of 0.3 to 7.0 cm (mean 1.58 cm). Symptoms are present in 4% to 9% of patients. The gender distribution is 1.5 to 4 times more frequent in men than in women. Symptomatic patients are usually young, in the cases exposed, both patients were male and it was observed that the diverticulum was located on the antimeenteric side of the ileum, approximately 80 cm from the ileocecal valve, with a length ranging from 2 to 10 mm. Therefore, the prevalence of gender, location, and length coincides with the range estimated in the research consulted (Hansen & Søreide, 2018).
Clinical presentation
Concerning clinical manifestations, case 1 was asymptomatic, which is consistent with what has been described in the literature. In contrast, case 2, a young patient, was symptomatic, which is also consistent with what was described by Hansen and Søreide (2018), it should be noted that the symptomatology was non-specific and after exploratory laparoscopy, the diagnosis of acute abdomen was established due to a Meckel’s diverticulum complicated with diverticulitis. This complicated clinical presentation is most frequently described in adults, as mentioned by Parvanescu et al. (2018), who highlight diverticulitis as the main complication of this disease. The main complaint in patients with Meckel’s diverticulum is usually abdominal pain. It is relevant to note that both patients initially shared this symptom as well as the diagnosis of appendicitis, a situation that, from the clinical point of view, as described by Chen et al. (2014), is because appendicitis and Meckel’s diverticulum share similar symptoms and clinical signs, such as fever, nausea, vomiting, tenderness and pain on pressure.
Diagnosis
Preoperative diagnosis was not possible in either case; however, this fact is consistent with what has been reported in the literature, where it is mentioned that most diagnoses are made incidentally. In one of the patients (Case 2) an exploratory laparoscopy was necessary to determine the cause of the disease, observing data of inflammatory reaction in the segment of the affected ileum, from the histopathological point of view this finding explains the origin of the symptomatology of Meckel’s diverticulum, causing an inflammatory process that resulted in diverticulitis.
Surgical Outcomes and Management
Surgical removal of Meckel’s diverticulum complicated with diverticulitis was performed in one of the patients, where the affected segment with end-to-end anastomosis was externalized and resected (see Figure 2). However, both patients were operated on successfully, achieving remission of symptoms and without observing any type of post-surgical complication, which evidences the effectiveness of this technique in both cases, also reflecting the experience and training of the surgical team involved, as well as the availability of resources and adequate technology for the procedure.
CONCLUSION
Correct diagnosis of complicated Meckel’s diverticulum in adults is difficult because the clinical features in adult patients presenting with complications are nonspecific and clinically indistinguishable from appendicitis. In the context of the Nicaraguan population, it is remarkable that two cases have been diagnosed in the same year, which is rare and underscores the rarity of this condition in this demographic group. Exploratory laparotomy seems to be an ideal surgical approach in cases of acute surgical abdomen with an uncertain diagnosis.
GRATITUDE
The authors thank the Ministry of Health of Nicaragua, Hospital Escuela Alemán Nicaragüense, medical-surgical team, anesthesia department, and patients for their generosity in allowing the use of their data for academic purposes.
DECLARATION OF INTERESTS
Conflict of interest
The authors have stated that they have no conflict of interest. Funding Source: This research did not receive any specific grants from funding agencies in the public, commercial, or nonprofit sectors.
Protection of people and animals
The authors state that no experiments have been carried out on humans or animals for this research and the surgical procedures were carried out with highly trained and certified personnel.
Ethical approval and confidentiality of data
During the hospital stay, verbal informed consent was obtained from the patients, who authorized the use of their clinical data after receiving a detailed explanation. They were assured that any personally identifiable information would not be exposed in this post. It is important to note that before any surgical intervention, the patients signed an official informed consent document, which is in the custody of the Archive Department of the Nicaraguan German Hospital, in this way the integrity and anonymity of the patients were guaranteed at all times, in this case report, which was carried out for purely academic purposes. On the other hand, it is worth mentioning that the approval of the patients was obtained for each study and intervention carried out during their stay in the hospital.
AUTHOR CONTRIBUTION
JAG-B: Idea conception, data collection, literature review, photo illustration, manuscript writing, final approval of manuscript version
FP-G: Manuscript writing, methodology, conception of ideas, literature review, final approval of the manuscript version.
work cited
Agha, Riaz A et al. “The SCARE 2020 Guideline: Updating Consensus Surgical CAse REport (SCARE) Guidelines.” International Journal of Surgery (London, England) vol. 84 (2020): 226-230. https://www.scareguideline.com/
Chen, J. J., Lee, H. C., Yeung, C. Y., Chan, W. T., Jiang, C. B., Sheu, J. C., & Wang, N. L. (2014). Meckel’s Diverticulum: Factors Associated with Clinical Manifestations. ISRN gastroenterology, 2014, 390869. https://doi.org/10.1155/2014/390869
Hansen, C. C., & Søreide, K. (2018). A systematic review of epidemiology, presentation, and management of Meckel’s diverticulum in the 21st century. Medicine, 97(35), e12154. https://doi.org/10.1097/MD.000000000001215
Murruste, M., Rajaste, G., & Kase, K. (2014). Torsion of Meckel’s diverticulum as a cause of small bowel obstruction: A case report. World journal of gastrointestinal surgery, 6(10), 204–207. https://doi.org/10.4240/wjgs.v6.i10.204
Parvanescu, A., Bruzzi, M., Voron, T., Tilly, C., Zinzindohoué, F., Chevallier, J. M., Gucci, M., Wind, P., Berger, A., & Douard, R. (2018). Complicated Meckel’s diverticulum: Presentation modes in adults. Medicine, 97(38), e12457. https://doi.org/10.1097/MD.0000000000012457
Shirakabe, K., & Mizokami, K. (2023). A Case of Torsion of Meckel’s Diverticulum. Cureus, 15(1), e33850. https://doi.org/10.7759/cureus.33850